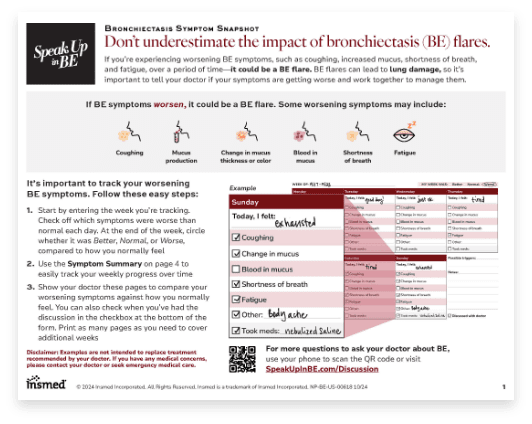
Bronchiectasis Symptom Snapshot
Share this tool with your patients to help them keep track of when their bronchiectasis symptoms get worse.
Goals in the management of bronchiectasis include disrupting the vicious vortex by addressing chronic airway infection, reducing chronic airway inflammation, enhancing mucociliary clearance, and mitigating lung destruction. 2-4
It’s important to take a multimodal treatment approach when you’re dealing with a patient with bronchiectasis, because there’s so many factors that are involved. We want to identify the potential etiology, the potential comorbidities to try to reduce the progression of the bronchiectasis. We want to try to reduce inflammation. You know, oftentimes, you know with airway clearance being a mainstay of that management, we want to try to treat infections and, you know, treat exacerbations and try to prevent exacerbations to really try to hinder the vicious vortex and prevent further progression of their bronchiectasis.
You know, we have multiple ways we can treat our patients with bronchiectasis, and if we reflect back on the vicious cycle and the vicious vortex, there are multiple places we can intervene to try to improve our patients’ symptoms and achieve all the objectives that we are trying to achieve. So we ought to be focusing on all the areas of the vortex to be able to optimize the management of our patients. And I know it’s hard to do that, but I think it’s important.
Targeting one aspect is not going to break the cycle in most patients, because it’s not just infection, or not just noninfectious inflammation, or not just problems with clearance of secretions. They all feed back on each other. So if you treat the retained mucus with airway clearance but you don’t treat the infection, you’re going to have an incomplete response. And vice versa, if you treat the infection and you don’t treat, say, underlying cause of inflammation, you’re still going to have dysfunction, ongoing inflammation, and all the negative effects of that.
Yeah, and a key part of what you’re describing there is people need to understand, this is a chronic condition. This is not like an acute pneumonia and antibiotics, it’s all going to be gone and they’re done. They’re going to have it for the rest of their lives. And so chronic illness requires chronic therapies, and so you need to have some kind of daily regimen to manage that.
All drivers of bronchiectasis should be targeted with a tailored approach to help address the interdependent modalities that may lead to devastating effects like exacerbations and disease progression. 4-6
Because bronchiectasis often appears alongside other diseases, patients should be assessed to identify potentially treatable underlying causes and comorbid conditions. 7-9
Bronchiectasis Symptom Snapshot
Share this tool with your patients to help them keep track of when their bronchiectasis symptoms get worse.

BE Action Plan
Fill out this resource with your patients to help them create an action plan for their bronchiectasis (BE), including treatment goals and what to do if they think they are having a bronchiectasis exacerbation.
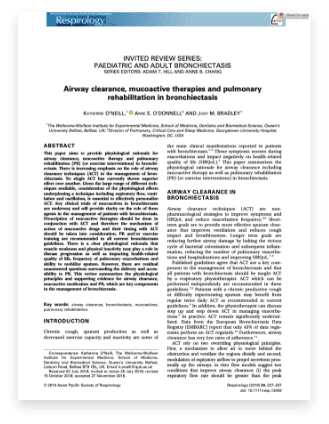
Airway clearance techniques and their benefits
Explore a publication with examples of airway clearance techniques, mucoactive therapies, and pulmonary rehabilitation in bronchiectasis.
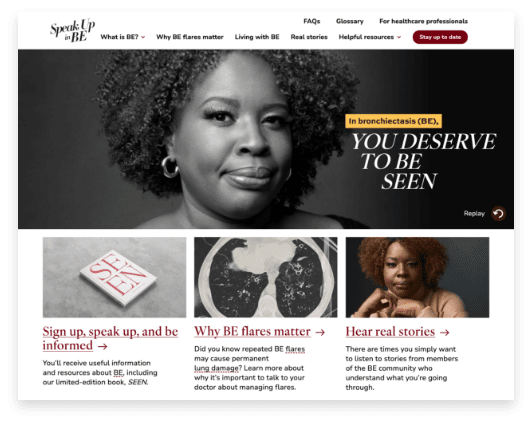
Speak Up In BE, a site for patients
See a website for people living with bronchiectasis (BE) to learn more about their disease, hear real patient stories, and find resources to help them manage their condition.

ATS Bronchiectasis Education Center
Explore a website for healthcare professionals that provides resources to help improve diagnosis and awareness of bronchiectasis progression.

Podcast library
Listen to audio content from CHEST about diagnosing and treating bronchiectasis.

The American Thoracic Society accelerates global innovation in the advancement of respiratory health through multidisciplinary collaboration, education, and advocacy.

The goal of Bronchiectasis and NTM 360 is to address the unmet needs of the bronchiectasis and nontuberculous mycobacterial (NTM) lung disease communities.

Bronchiectasis Info and Research was developed to provide information and support to patients with bronchiectasis by promoting early diagnosis, improved treatments, and research.

Through advocacy, education, and research, the American Lung Association improves the lives of people living with bronchiectasis.
Get answers to frequently asked questions about bronchiectasis.